Overview
A uterine fibroid is the most common benign (not cancerous) tumor of a woman's uterus (womb). Fibroids are tumors of the smooth muscle that is normally found in the wall of the uterus. They can develop within the uterine wall itself or attach to it. They may grow as a single tumor or in clusters. Uterine fibroids can cause excessive menstrual bleeding, pelvic pain, and frequent urination; so even though they are termed "benign (not cancerous) tumors," fibroids potentially can cause many health problems.
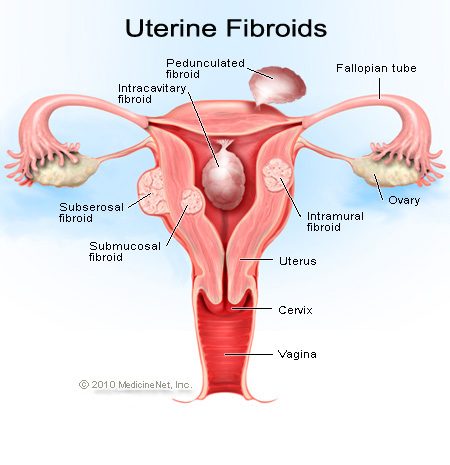
- Fibroids start in the muscle tissues of the uterus. They can grow into the uterine cavity (submucosal), into the thickness of the uterine wall (intramuscular), or on the surface of the uterus (subsersoal) into the abdominal cavity. Some may occur as pedunculated masses (fibroids growing on a stalk off of the uterus).
- Although these tumors are called fibroids, this term is misleading because they consist of muscle tissue, not fibrous tissue. The medical term for a fibroid is leiomyoma, a type of myoma or mesenchymal tumor.
Uterine Fibroid Causes
The exact reasons why some women develop fibroids are unknown. Fibroids tend to run in families, and affected women often have a family history of fibroids. Women of African descent are two to three times more likely to develop fibroids than women of other races.
Fibroids grow in response to stimulation by the hormone estrogen, produced naturally in the body. These growths can show up as early as age 20 and shrink after menopause when the body stops producing large amounts of estrogen.
Fibroids can be tiny and cause no problems, but they also can grow to weigh several pounds. Fibroids grow slowly.
The following factors have been associated with the presence of fibroids:
- Being overweight, obesity
- Never having given birth to a child (called nulliparity)
- Onset of the menstrual period prior to age 10
- African American heritage (occurring 3-9 times more often than in Caucasian women)
Uterine Fibroid Symptoms
Most fibroids, even large ones, produce no symptoms. These masses are often found during a regular pelvic examination.
When women do experience symptoms, the most common are the following:
- irregular vaginal bleeding or an increase in menstrual bleeding, known as menorrhagia, sometimes with blood clots;
- pressure on the bladder, which may cause frequent urination and a sense of urgency to urinate and, rarely, the inability to urinate;
- pressure on the rectum, resulting in constipation;
- pelvic pressure, "feeling full" in the lower abdomen, lower abdominal pain;
- increase in size around the waist and change in abdominal contour (some women may need to increase their clothing size but not because of a significant weight gain);
- infertility, which is defined as an inability to become pregnant after 1 year of attempting to get pregnant; and/or
- a pelvic mass discovered by a health care practitioner during a physical examination.
When to Seek Medical Care
If a woman has any questions about her uterine health, seek medical assistance as soon as possible. If a woman has any of the following, she should notify her health care practitioner:
- Irregular or heavy menstrual cycle, bleeding between periods
- Pelvic or abdominal pain
- Fever or night sweats
- Increasing abdominal girth
- Concerns about pregnancy or inability to become pregnant
If a woman has any of the following signs or symptoms she should contact a health care practitioner immediately or go to a hospital's emergency department.
- Menstrual bleeding soaking through more than 3 pads per hour
- Severe or prolonged pelvic or abdominal pain
- Dizziness, lightheadedness, shortness of breath, or chest pain associated with vaginal bleeding
- Vaginal bleeding associated with pregnancy or possible pregnancy
Uterine Fibroids Diagnosis
A woman's health care practitioner will discuss her medical history and conduct a physical examination that includes a pelvic exam. Often a doctor can feel an irregularly shaped uterus when fibroids are present.
If further studies are indicated, the doctor may choose one of the following tests to help decide if the patient has fibroids and to exclude other and potentially more serious causes of ongoing symptoms:
- An abdominal, transvaginal or pelvic ultrasound can help identify the number, size, and shape of most fibroids. These test use sound waves to give doctors an image of the pelvic area. A wand is passed over the abdomen (abdominal ultrasound) for one type of view. Another probe (or wand) may be inserted into the vagina to obtain additional views (pelvic or transvaginal ultrasound).
- An endometrial biopsy is performed by taking a tissue sample from the uterus. A small instrument is passed through the cervical opening to "grab" small samples of tissue inside the uterus. It can be performed at a doctor's office.
- A hysteroscopy looks at the uterus by passing a small fiberoptic camera through the opening of the cervix.
- Hysterosalpingography involves injection of dye into the uterus and Fallopian tubes, which is then X-rayed to identify the anatomy of these structures.
- Laparoscopy is a surgical procedure. The surgeon will insert a small fiberoptic camera into the abdomen through small abdominal incisions to look directly at internal organs.
Surgery
Surgery options for treatment have both risks and benefits. Be sure to discuss these risks and benefits with the doctor. Some treatment options may not be right for a woman because of the characteristics of the fibroids or other health factors.
- Myomectomy is the surgical removal of the fibroids only. This can be accomplished through hysteroscopy, laparoscopy, or, less frequently, an open procedure (an incision in the abdomen). The surgical approach depends on the size and location of the fibroid. Pretreatment with GnRH analogs has been shown to decrease blood loss and operative time in women undergoing myomectomy. Myomectomy has also been shown to have a decreased likelihood of injury to the bowel, bladder, or ureter than hysterectomy. The uterus is left intact in this type of procedure, and the patient may be able to become pregnant.
- Hysterectomy is the surgical removal of the uterus (and fibroids). It is the most commonly performed surgical procedure in the treatment of fibroids and is considered a cure. Depending on the size of the fibroid, hysterectomy can be performed with incisions through the vagina or abdomen. In some cases the procedure may be performed using laparoscopy. Use of GnRH agonists can reduce the size of the fibroid to allow less invasive surgical techniques. In past experience, less blood loss has occurred using hysterectomy than myomectomy. But this may change as preoperative hormone treatment is improved and blood loss is reduced because hormone use helps the tumors shrink. Hysterectomy with removal of the Fallopian tubes and ovaries (called a salpingo-oophorectomy) may be indicated if there is suspicion of cancer or if ovarian masses are present.
- Uterine artery embolization, or clotting of the arterial blood supply to the fibroid, is an innovative approach that has shown promising results. This procedure is done by inserting a catheter (small tube) into an artery of the leg (the femoral artery), using special X-ray video to trace the arterial blood supply to the uterus, then clotting the artery with tiny plastic or gelatin sponge particles the size of grains of sand. This material blocks blood flow to the fibroid and shrinks it. This method may prove to be a good option for women if other methods have not worked, she does not want surgery, or may not be good candidates for surgery. A specialist known as an interventional radiologist performs this procedure.
|